A groundbreaking study, led by Professor Yvonne Nolan of the APC Microbiome Ireland research center, has revealed a fascinating connection between Alzheimer’s disease and gut microbiota. The international collaboration behind this research aims to shed light on the early stages of dementia, potentially paving the way for new therapies and personalized interventions.
In the study, 69 patients with Alzheimer’s disease and 64 control subjects were recruited. Blood and stool samples were collected from each participant. The stool samples underwent a procedure called fecal microbiota transplantation (FMT), which involves transferring gut microbes to another organism. In this case, young adult male rats were the lucky recipients, chosen to eliminate the effects of natural aging.
After pretreating the rats with antibiotics to deplete their own microbiota, FMT was performed. Ten days later, the rats underwent behavioral tests, and samples of their gut tissues, brain tissues, blood, and feces were collected for analysis.
The results were astonishing. The human patients had higher levels of inflammation-promoting bacteria in their fecal samples, which correlated with their cognitive impairment. When these gut microbes were transferred to the rats, they developed symptoms associated with dementia.
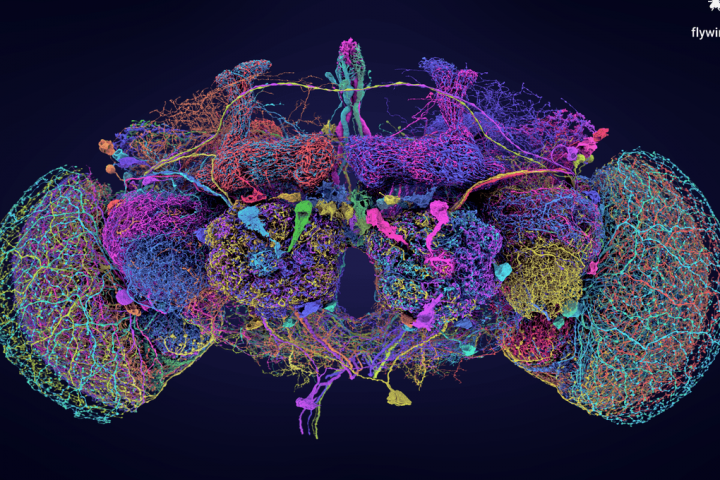
One of the key findings highlighted by the researchers was the impact on adult hippocampal neurogenesis, the birth of new neurons in the hippocampus, a region vital for learning and memory. Animals with gut bacteria from Alzheimer’s patients produced fewer new nerve cells and experienced impaired memory.
The team also confirmed their findings in human cell cultures, demonstrating that serum from Alzheimer’s patients impaired the growth and functioning of these cells.
The gut microbiome has gained significant attention in recent years, with implications for various aspects of human health. Alzheimer’s disease, the most common form of dementia, could affect one in three people born today if current trends continue. Therefore, a better understanding of the disease’s pathology and new treatment approaches are urgently needed.
Professor Sandrine Thuret, a neuroscientist at King’s College London and one of the study’s senior authors, emphasized the importance of this research, stating, “This study represents an important step forward in our understanding of the disease, confirming that the make-up of our gut microbiota has a causal role in its development.”
The study, published in the journal Brain, has laid the groundwork for future research in this area, offering hope for potential advances in therapeutic interventions.