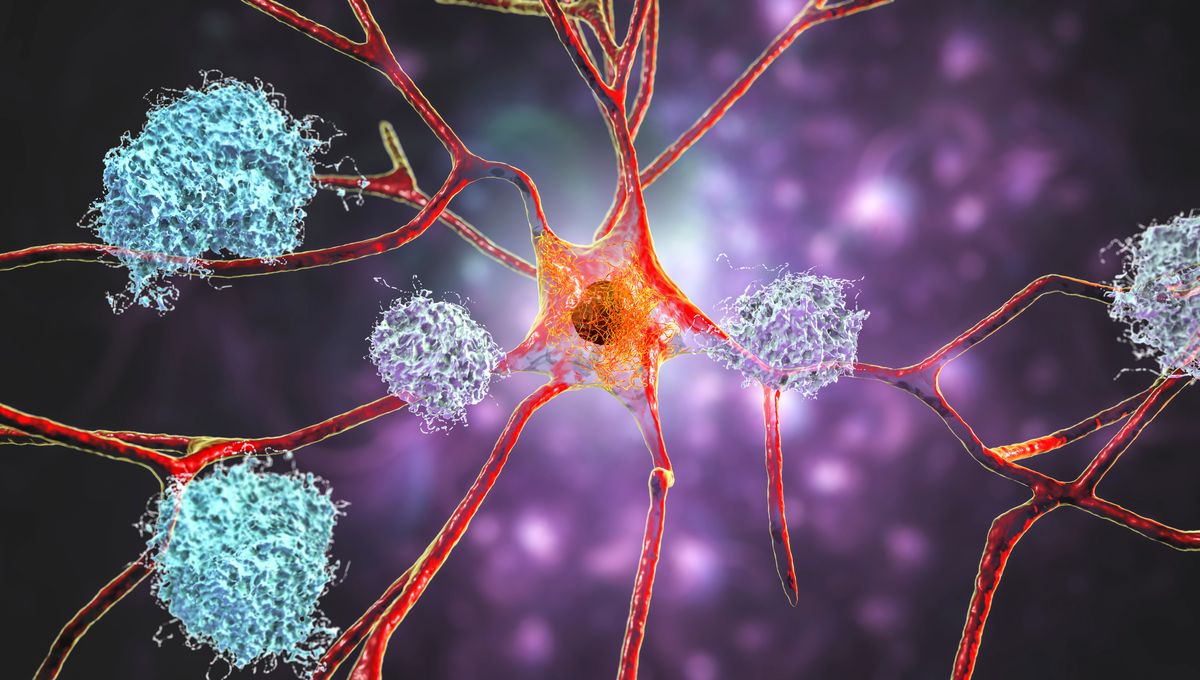
The “amyloid hypothesis” suggests that the accumulation of amyloid-beta protein is responsible for the degeneration and death of neurons in Alzheimer’s disease. Over a century ago, unidentified protein plaques were found in the brain of a person with dementia. In 1984, amyloid-beta protein was discovered and remains a key suspect in the development of Alzheimer’s.
However, since these plaques are also present in the brains of elderly individuals with normal cognitive function, and because treatment development has struggled for years, some have questioned the validity of this hypothesis. There have even been allegations of evidence fabrication in a highly influential paper supporting the theory last year. Additionally, the two most recent trials do not seem to support it either.
These trials, involving nearly 1,000 participants, tested a drug called gantenerumab in individuals with early Alzheimer’s disease. While the treatment did reduce amyloid plaque burden compared to a placebo, there was no improvement in cognitive function as expected.
This is “surprising,” according to Lon Schneider in an accompanying editorial. Gantenerumab is similar to two other FDA-approved drugs, aducanumab and lecanemab, for early Alzheimer’s treatment. All three drugs contain synthetic antibodies that bind to amyloid-beta in the brain to reduce plaques. However, whether this leads to improvements in dementia symptoms is debated, especially in light of the latest findings.
Participants were randomly assigned to receive gantenerumab or a placebo every two weeks for 116 weeks. The researchers used the Clinical Dementia Rating scale–Sum of Boxes (CDR-SB) to assess dementia severity before and after the trials. After over two years, there was no significant difference in CDR-SB score changes between the drug and placebo groups, indicating that gantenerumab did not significantly improve cognition.
“The gantenerumab trials add to the evidence of variable, small clinical effects of antiamyloid antibodies. Depending on one’s perspective, the results either reinforce confidence in this therapeutic approach or suggest that the effects are small, unreliable, and barely distinguishable from no effect,” concludes Schneider.
However, Schneider also acknowledges some limitations of the trials, including bias risk and inadequate masking of the drug and placebo. He suggests that the trials may not have been long enough to observe a real difference in Alzheimer’s symptoms.
“If a meaningful effect is not apparent after 1.5 to 2 years of treatment, there may be hope that it manifests in the future,” Schneider adds.
After decades of research on the role of amyloid plaques in Alzheimer’s development, a definitive answer will still have to wait.
“There is much we do not know about targeting amyloids in patients with Alzheimer’s disease, and perhaps we will learn more from ongoing prevention or registry trials of antiamyloid antibodies in clinical practice,” says Schneider.
The results of the trials are published in The New England Journal of Medicine.